By Victoria Dames, Vice President of Product Management, Identity and Optimization
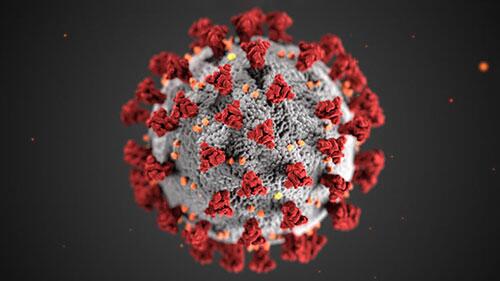
As we continue to emerge somewhat fitfully from the pandemic, the healthcare industry faces unprecedented data challenges related to volume, telehealth and digital front door initiatives. The excess data flowing through new workflows present patient matching issues and the potential for disparate medical records. Add to that another broad and potentially chronic data challenge relating to diagnosing, treating and managing costs from sufferers of long COVID-19.
We know from a recent Penn State study that half of patients who recovered from symptomatic infections suffer symptoms for at least six months after recovery, and according to a Swedish study approximately 10% of patients who had mild cases experienced one moderate to severe symptom eight months post-recovery. To put that in perspective, there have been some 45 million COVID cases reported in the US, while the CDC estimates that the actual number of cases in the US between February 2020 and May 2021 was more than 120 million.
Diagnosing symptoms among this vast patient population represents an immense clinical challenge, as long COVID isn’t a disease but rather a loose collection of ailments that can range from heart and lung issues to hair loss, skin rashes and a host of difficulties related to digestion, concentration and well-being. According to the American Medical Association (AMA) and the CDC, even people who did not have any COVID symptoms can experience long COVID, which can present as different types and combinations of health problems and can range in lengths of time.
Now, as of Oct. 1, there is a new diagnosis code – Code U09.9 (Post COVID-19 condition, unspecified) – which enables providers to establish a coding link between the coronavirus and lingering symptoms after the virus is no longer active. The CDC advises that providers should list U09.9 secondary to specific codes for lingering conditions such as chronic respiratory failure, loss of smell, loss of taste, multisystem inflammatory syndrome, pulmonary embolism and pulmonary fibrosis. The code is not to be reported for active COVID cases, except when there is a re-infection that occurs with a condition related to prior COVID-19.
Costs and reimbursements for long COVID care are also uncertain, especially now that the government and insurers are letting their emergency coverage and cost-sharing programs expire. Patients may not know what they can afford to treat and therefore avoid diagnoses in the first place or following treatment, learning they have expenses they cannot cover. This has collection and revenue implications for providers who’ve already been hit hard by the pandemic.
Finally, there’s the continuing evolution of how and when people access their healthcare, as access to telehealth, pharmacy clinics and wearables is generating huge amounts of data that could be relevant to diagnoses and treatment of long COVID if they could be reliably gathered and applied to patient records. This digitalization of healthcare was happening before the pandemic, was supercharged by it and is not going to stop, yet we have no established ways to manage it.
There’s been talk of a “Generation C” of patients who’ve only known the world after COVID, and this world is already awash with vast amounts of data and tens of millions of patients who would benefit from its effective use.
So, what can we do to meet this challenge? First, redouble our efforts to make sure patient records are accurate, so that lingering and easily fixable errors of name or address don’t make it even harder to capture new data and also provide the ability to keep one holistic patient record. Second, providers can establish their own classification standards to add to existing fields of information and ensure that data are captured consistently (this can include noting incidences, whether reported or suspected, of COVID). Third, providers and patients can work more closely and openly on identifying coverage options at the start of healthcare journeys, not just when costs have already been incurred.
The diagnosis is clear: The data challenge of treating long COVID is upon us. How we treat it is up to us.
The Editorial Team at Healthcare Business Today is made up of skilled healthcare writers and experts, led by our managing editor, Daniel Casciato, who has over 25 years of experience in healthcare writing. Since 1998, we have produced compelling and informative content for numerous publications, establishing ourselves as a trusted resource for health and wellness information. We offer readers access to fresh health, medicine, science, and technology developments and the latest in patient news, emphasizing how these developments affect our lives.