Photo credit: Depositphotos
By Nick Macario, CEO of Verifiable
Andreessen Horowitz, also known as a16z, is one of the most well-known venture capital firms in Silicon Valley, and for good reason. With investments in such notable exits as Airbnb, Facebook, Box and Slack – Andreessen Horowitz has regularly been at the forefront of software trends disrupting traditional industry. With over $1.4Bn in its bio funds, a16z has a clear focus on remaining on the forefront of the rapid innovation occurring within the digital health space.
Notably, Julie Yoo, general partner at a16z with a focus on healthcare, recently issued a report defining “The New Tech Stack For Virtual First Care,” calling out new, API-first solutions that are helping telehealth companies rapidly build more scalable, efficient operations.
Here at Verifiable, we’re thrilled to be called out as one of the notable companies listed in the a16z report currently powering virtual care companies, and are energized to have our API-first approach to provider credential verification and monitoring further validated by industry thought-leaders.
Digital Health Continues To Surge
Tracking the recent growth in the overall digital health market, Yoo points out that 2020 was a record-breaking year in the number of digital health companies that got started and funded, as well as the extensive growth these platforms achieved in both patient utilization and revenue. In the a16z analysis, Yoo finds that more than 1,000 full-stack digital health companies have been started in the past three years, and believes “we’re truly entering into a new golden era for healthcare technology”
The staggering growth seen within the health-tech space is further captured in CBInsights recent State of Healthcare: Sector and Investment Trends to Watch report, which finds calls out that global digital health funding jumped 45% YoY in 2020, with telehealth startups raising over $10B in 2020 (and a record $3.3B in funding in Q4’20 alone).
Legacy Healthcare IT Fails To Deliver for Digital Health
New virtual care companies require much of the same back-end infrastructure as traditional healthcare providers, however legacy healthcare IT solutions continue to lack the flexibility, interoperability, and ability to scale that the category requires. Therefore, to date, many digital health companies have needed to pursue the costly endeavor of building their tech stacks in house or fully outsource to costly manual operations.
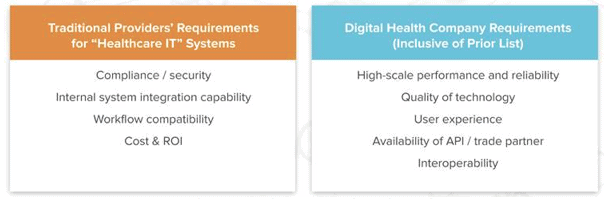
(Image source from “New Tech Stack of Virtual Care Delivery”, Andreessen Horowitz)
The Rise of The “New Tech Stack for Virtual First Care”
According to Yoo,“In the same way that Plaid, Stripe and AWS abstracted out entire layers of infrastructure and dramatically reduced the cost and time to stand up a new tech business, these health-tech companies are now allowing digital health startups to accelerate their time to market and really focus on the higher-order elements of their products and services to deliver game-changing care to patients.”
Fortunately, strong growth in the digital health sector has spurred the rise of a new wave of health technology infrastructure, what Yoo dubbed as “‘The New Tech Stack for Virtual First Care.”
Solutions in this new stack span across the front office, clinical, and back office operations. By providing flexible, scalable API-first offerings, digital health companies can easily integrate and configure them to fit their needs, tipping the scales of the “buy vs. build” decision. This allows telehealth companies to reinvest realized efficiencies and cost-savings back into delivering great care and value for their end users.
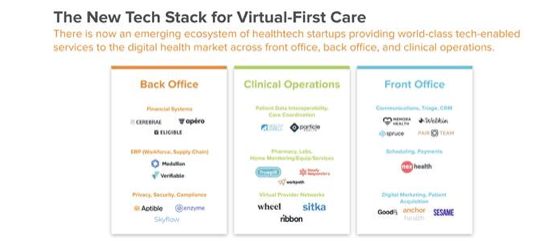
(Image source from “New Tech Stack of Virtual Care Delivery”, Andreessen Horowitz)
APIs To Supercharge Provider Data Management
A major pain point for both virtual first care and traditional healthcare delivery alike has been the tedious status quo for verifying provider licenses and credentials. Manual, time-consuming, one-by-one style workflows have typically required healthcare organizations to build out teams of operational staff to manage these processes, often with limited effectiveness. License verification and credentialing workflows workflows often become bottlenecks with long turnaround times, limiting ability to scale with volume and magnets for risk as regulations change or continued follow-up is needed.
In partnering with leading telehealth and virtual care companies here at Verifiable, we’ve seen three key areas in which more flexible APIs for provider credential verification and monitoring have had the most immediate impact.
Provider Onboarding
The “Old Way”: Intake of provider data has historically been excruciatingly within the traditional healthcare space, usually still involving paper, fax machines, or at best multiple email communications. While many digital health and virtual care providers have modernized this process through using flexible, lightweight onboarding forms like Google Forms and Survey Monkey to capture data, these forms do little to catch entry errors upfront, require endless entry fields and still result in the data existing outside core systems of record.
The “New Wave”: With API-first data solutions like Verifiable embedded into onboarding forms, provider data can be quickly pre-populated from an NPI or SSN, greatly reducing friction within the provider onboarding process and minimizing the risk of poor data entry (that will cause significant delays later). Lightweight, real-time data verifications of the data can even be embedded directly into these forms, providing immediate feedback and prompts to busy providers right in the same session to update incorrect information. This validated data from these verifications can now also be re-used without cost throughout subsequent processes like network approval, credentialing or enrollment.
Credentialing and Enrollment
The “Old Way”: This tedious process either required healthcare organizations to work with slow, expensive, inflexible outsourced solutions where they had little control over their own data, or build out teams in-house to manually perform one-off primary source lookups across disparate data sources, track any changes and compile results in a compliant manner.
The “New Wave”: Now starting with high-quality, validated data flowing from onboarding, fast-growing healthcare organizations are using modern solutions, leveraging its powerful data-matching algorithms to automate primary source verifications across hundreds of sources and obtain instant results. Beyond the digitized data populating directly in core systems of record, screenshots and audit logs are also auto-captured to meet the highest levels of NCQA compliance. With complete control over their provider data digitized and integrated within core platforms, modern healthcare companies can now develop advanced reporting and tooling or further automate and streamline provider enrollment activities.
Provider Network Monitoring
The “Old Way”: Tickler files, calendar reminders or it simply falling through the cracks, ongoing monitoring of provider networks has historically been a time-consuming and haphazard process at best. It either is a complete resource drain and disruptor for in-house teams, or an expensive black box with little visibility or quality control when outsourced. As telehealth grows and further depends on a distributed provider network to deliver greater access to care, so does the criticality for these companies to maintain and monitor their quickly evolving provider networks.
The “New Wave”: With the fast pace that many telehealth and virtual care companies are moving, they’re looking for flexible API-first solutions that can keep pace with and integrate directly into their operations. By piping directly to hundreds of primary sources, sanctions and exclusions, DEA, OIG, SAM and other sanctions and exclusions lists, newer monitoring solutions can now deliver instant alerts as statuses change or issues arise.
Again, robust APIs here are key as it allows these alerts to be delivered directly into the core systems the operations team is already using most. Similar to a tree falling in the woods, is alert any good if it happens in a platform that no one is ever in?
Wrapping Up
Healthcare has fast forwarded 10 years worth of advancement in a matter of 10 months, which has allowed for many of the 1,000 recently formed digital health startups to quickly gain traction, as well as more established players capitalize. Though, only now is the telehealth sector achieving the critical mass necessary to support this ‘new wave’ of modern healthcare infrastructure that enables (versus hamstrings) the efficient delivery of virtual first care.
One particular area of this tech stack that has remained time-consuming, unreliable and highly inefficient has been in the end-to-end workflows related to provider onboarding, credentialing, and network monitoring. Though, a “new wave” of API solutions to verify and monitor provider data seamlessly integrating throughout core workflows are creating the back-end infrastructure to help digital health companies effectively scale to meet demand, deliver a better provider experience and unlock new possibilities through flexible, digitized data.
The Editorial Team at Healthcare Business Today is made up of skilled healthcare writers and experts, led by our managing editor, Daniel Casciato, who has over 25 years of experience in healthcare writing. Since 1998, we have produced compelling and informative content for numerous publications, establishing ourselves as a trusted resource for health and wellness information. We offer readers access to fresh health, medicine, science, and technology developments and the latest in patient news, emphasizing how these developments affect our lives.








