It’s the classic chicken and the egg problem. Which came first, data or personalization? Patients want personalized experiences, but many are uncomfortable sharing the data needed to deliver these experiences. This is a conundrum we have been studying for the last six years.
In developing journey maps for the future of healthcare across acute care, chronic conditions, and wellness, it’s clear that people want smart, personalized, and even genius solutions to help them improve their health and wellbeing. In fact, over eighty percent of people want to engage with digital tools that truly enable them to better their health, and over half of people use digital tools and devices to help them today.
So why do many not feel safe sharing their data, and why do so many tools fail to deliver on their promises?
Key Challenges
- Fear of data being used against them or inappropriately – Patients are skeptical about company motives for collecting data and concerned that their health data could be used against them to charge more for things such as health insurance premiums; to shame them about their health challenges; or to make money through selling their data to unapproved sources (thank you, Facebook).
- Burden of data collection & integration – In order to create a valuable digital health tool, data is often needed from disparate sources ranging from a patient’s own personal devices to their health records that may exist across multiple health systems in different EMRs. The burden of this still very manual task often falls on the patient themselves – or their caregiver – and becomes even more challenging if the patient is very ill. Even with the new 2022 regulation granting patients access to their digital health records, access and interoperability challenges remain. While strides are being made, it is still hard to pull data from one EMR, device, or app into another one to easily understand and see a holistic picture of health.
- HCP Experience – The usability of the data generated from these tools largely depends on the HCP’s trust in the clinical relevancy and validity of the data, which is still low for personal wearable data. With HCPs often having an average of 12 minutes with patients, ensuring that the data collected from digital health tools fit into their clinical workflow is critical for its success.
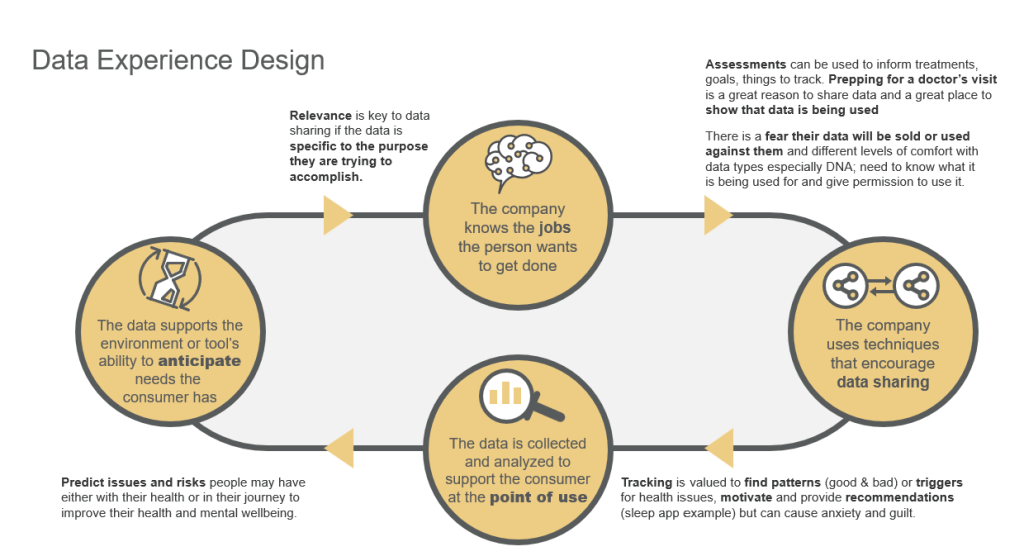
- Lack of Good Data Experience Design Principles – The biggest issue is that many digital healthcare experiences don’t leverage data experience design principles for the patient or HCP. From our research in the Digital Healthcare Collaborative, the quickest way to make patients feel safe is to show them value for their data. Show that you deeply understand their jobs to be done (what they are hiring you to do), that you value their goals and their health story, and that you are using their data to support them when and where they need support, and ideally use the data to anticipate any health issues or flare-ups they may have.
Techniques for Creating a Good Data Design Experience for Patients & HCPs
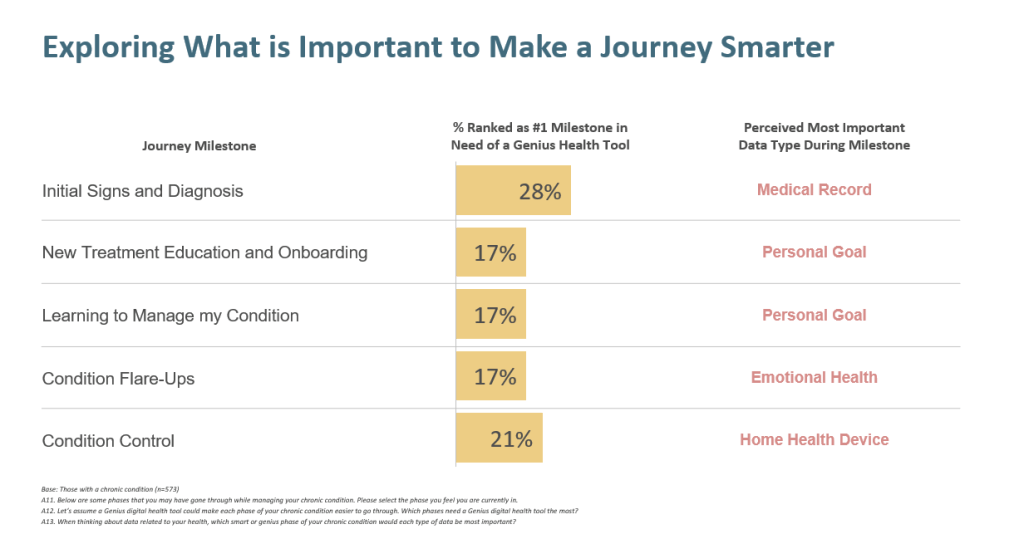
This starts with understanding the healthcare journey and what data is important when. In our research on the chronic health journey, people most want their data to be used to support initial diagnosis and ongoing condition control, but data is also important for improving onboarding to the condition, learning to manage it, and managing flare-ups. The type of data they see as most important varies by the phase of the journey, though.
Not surprisingly, the medical record is most important for initial diagnosis, but their personal goal data matters most for onboarding and learning to manage their condition, home health device data is most critical for ongoing condition management, and emotional health data for condition flare-ups. Apple’s recent announcement on their AI-Powered mood tracker, iPad health app, and coaching service may provide the type of genius tool that patients are looking for to help them manage emotional setbacks that come with flare-ups.
Once you understand how to deliver on key jobs to be done by patients, like shortening the time to initial diagnosis, individualizing onboarding, or increasing condition control, leverage key data-sharing techniques to build trust in data sharing. We’ve identified eight key techniques, and a few of them are:
- Demonstrate informed care delivery – One technique is to show patients how their care decisions will be more informed over time, how their healthcare team will use the data, and how it will be summarized to help their doctor. Patients know they don’t remember everything, and they want to ensure their fifteen minutes with the doctor are productive. Improving the data used in their doctor’s appointments for condition management is a great way to make people feel that sharing their data is worth it.
- “Know-you” Curation – Another great technique is “know you curation.” Show patients how their data will personalize their onboarding, learning, and ongoing communication around their health condition or goals. Make it easy to share their goals and health story through quick quizzes or assessments (even visual ones). Then use this data to curate condition content, reminders, and fun nudges. The more you use the data to support health goals in day-to-day life, the safer patients will feel sharing data.
- Measure milestones & progress – Two data-sharing techniques can work together to add value for patients. Anything that can be measured can be broken into milestones. When you ask about health goals (the data patients feel is most important for condition onboarding), you can build in milestones, both micro and meaningful, to help people see progress, stay the course, and achieve their health and wellness goals. Tracking is a way of getting credit for the sharing of their data.
- Life Configuration – When we were trying to explore smart and genius healthcare experiences, we asked people about the health superpowers they most want companies and their data to support for them. There are eight key superpowers they want to be enabled, but health prediction and life configuration are the top two. Both of these superpowers require a lot of data to deliver. Once milestones are set, you can ask for the data to help fit them into a person’s life. Having that personalized data will improve the value of the content and nudges you provide and the likelihood of success for the patient.
Knowing that you are HIPPA compliant provides a sense of security and safety for data, but what really encourages data sharing and builds trust is making it easy for the patient to get value from the data they are sharing with you. Use their data to show empathy, encourage intentionality, and deliver on their jobs to be done.
Dave Norton, Ph.D. is the Founder and Principal of Stone Mantel, a research-led consultancy at the forefront of customer and employee experience strategy. With the support of lead experience strategists like Mary Putman, they guide, research, and build frameworks to help companies like Marriott, US Bank, Best Buy, and Clayton Homes deliver on Time Well Spent for customers and employees. Learn more at https://www.stonemantel.co/.







