When it comes to Nonalcoholic Fatty Liver Disease (NAFLD), there’s nothing but devastating statistics.
According to the American Liver Foundation:
- It’s the number one cause of chronic liver disease.
- An estimated 100 million Americans – including children – have NAFLD.
- It’s the third most common reason for liver transplants.
But what is Nonalcoholic Fatty Liver Disease?
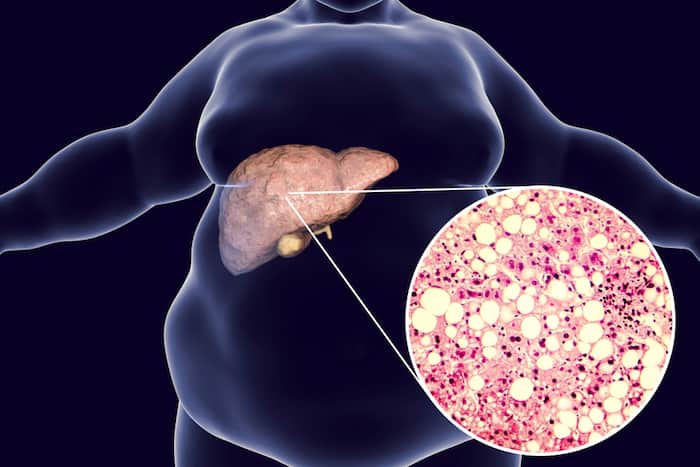
As its name implies, Nonalcoholic Fatty Liver Disease (NAFLD) is a medical condition wherein the liver accumulates excess fat that’s not from high and prolonged alcohol consumption.
What causes NAFLD?
It’s still unknown what causes NAFLD. However, experts agree that people who suffer from obesity, diabetes, and high cholesterol are the most commonly diagnosed with it.
Other factors that may increase the risks of NAFLD include:
- Genetics or hereditary influences
- Old age
- Smoking
- Toxin exposure
- Certain medications (e.g., steroids and cancer treatment medications, like tamoxifen)
- Rapid weight loss
- Liver infections (i.e., hepatitis)
What are the symptoms of NAFLD?
Currently, there isn’t a definitive set of symptoms that’s exclusive to NAFLD, which makes early detection extremely difficult.
So unfortunately, NAFLD often goes undetected until it turns into its more severe form called nonalcoholic steatohepatitis (NASH). At this stage the liver is already swollen, and in most cases, already requires a transplant.
Some of the symptoms you should watch out for include:
- Fatigue
- Swollen stomach (Swelling is most evident in the upper right hand of your stomach where your liver is located.)
- Extreme weight loss
- Enlarged breasts for men
- Jaundice
- Mental confusion
If you’re experiencing any of these symptoms and suspect you may have Nonalcoholic Fatty Liver Disease, consult your doctor immediately.
How is Nonalcoholic Fatty Liver Disease diagnosed?
The most common way to diagnose NAFLD is through a blood test.
- Using a liver function test, NAFLD can only be diagnosed after all other liver conditions are first identified and excluded.
- Keep in mind however, that blood tests aren’t 100% accurate in detecting NAFLD.
If you’re overweight, doctors recommend regularly getting a liver function test to determine and monitor your liver enzyme levels.
When a blood test fails to detect NAFLD but there’s still a strong suspicion of its presence, specialists would often recommend getting a computed tomography (CT) scan or ultrasound.
- Clearly shows the amount of fat in the liver through imaging technology.
- In some cases, a specialized ultrasound called Fibroscan can also be used.
However, if you want accurate results, a liver biopsy is still the most reliable way to diagnose NAFLD.
- A small needle is inserted in the area of your abdomen where your liver is located to acquire a sample of your liver for testing.
- A biopsy shows more detailed information on the condition of your liver as compared to blood testing and ultrasound.
How does NAFLD progress?
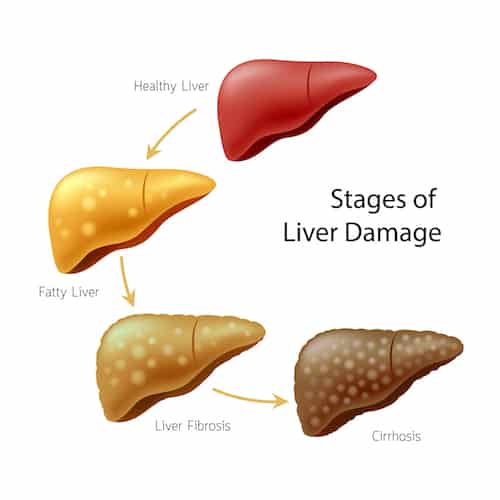
There are different stages to Nonalcoholic Fatty Liver Disease:
Simple Fatty Liver or Steatosis
This liver condition is generally harmless. It involves fat buildup in the liver cells. Usually, this condition is accidentally diagnosed when tests are carried out for another medical condition.
Non-alcoholic steatohepatitis or NASH
As compared to simple fatty liver, this is a more serious type of NAFLD, wherein the liver becomes inflamed.
From the fatty liver, continuous fat accumulation may cause inflammation of the liver, causing nonalcoholic steatohepatitis or NASH.
This liver condition affects about 3 to 12 percent of adults in the United States, and about 75% suffer from hepatomegaly or swelling of the liver.
The signs and symptoms of NASH are vague because they may resemble other medical problems. That’s why laboratory tests and imaging studies should be carried out to diagnose the real condition of the patient.
Here are the signs and symptoms of NASH:
- Muscle weakness
- Lack of energy
- Easy fatigability
- Swelling of the upper abdomen
- Decreased appetite
- Weight loss
- Nausea
- Pain or discomfort of the abdomen
Fibrosis
Scarring of the liver occurs at this point due to persistent inflammation. While scar tissue occurs around the liver and its nearby blood vessels, the liver may still function normally.
When diagnosed immediately and treatment is quickly administered, there’s a very good chance that your liver can heal itself.
Liver Cirrhosis
It is considered as the most severe stage of NAFLD, wherein it occurs after years of inflammation and no treatment.
The liver tissue shrinks, becoming scarred and lumpy, causing permanent liver damage that can lead to liver failure.
In normal liver condition, this organ removes waste products, like medicines and toxins from the body.
But when liver cirrhosis strikes, the scar tissue impedes blood flow, and the liver stops functioning the way it should.
Here are the signs and symptoms of liver cirrhosis and liver failure:
- General weakness
- Easily fatigued
- Nausea and vomiting
- Diarrhea
- Tarry stools
- Jaundice or yellowish color of the sclera or white part of the eye
- Abdominal swelling
- Ascites
- Abdominal pain
- Bleeding and bruising
- Spider-like veins in the skin
- Confusion (due to blood toxin buildup), memory loss, poor concentration, and hallucinations
- Kidney problems
- Weight loss
Lifestyle modification is important if you’re diagnosed with NAFLD to avoid developing liver fibrosis and cirrhosis.
How can NAFLD be prevented?
Although it might sound trite, NAFLD can be prevented by – regular exercise and eating a healthy, balanced diet.
In fact, recent research has found that increasing healthy gut bacteria found in vegetables can benefit people with NAFLD.
According to data from the study, adding more cruciferous vegetables (e.g., cabbage, kale, cauliflower, Brussels sprouts) in your diet can help combat NAFLD.
Conclusion
During the first stage of nonalcoholic fatty liver disease, the patient won’t feel any symptom or show any sign of a liver problem.
However, as fat accumulates, the liver becomes inflamed (non-alcoholic steatohepatitis or NASH), and scarring occurs, which causes fibrosis, manifested by tiredness, loss of energy, weight loss, and decreased appetite.
Over time, if appropriate medical treatment is not implemented, the liver ceases to function properly, and the patient would show signs and symptoms of liver cirrhosis and liver failure.
At this point, jaundice is an evident or yellowish tinge of the skin and the sclera of the eye and bruising or bleeding.
Also, the patient becomes confused and restless due to the accumulation of toxins in the blood, affecting focus and cognitive functioning.
The Editorial Team at Healthcare Business Today is made up of skilled healthcare writers and experts, led by our managing editor, Daniel Casciato, who has over 25 years of experience in healthcare writing. Since 1998, we have produced compelling and informative content for numerous publications, establishing ourselves as a trusted resource for health and wellness information. We offer readers access to fresh health, medicine, science, and technology developments and the latest in patient news, emphasizing how these developments affect our lives.







