By Linda Comp-Noto
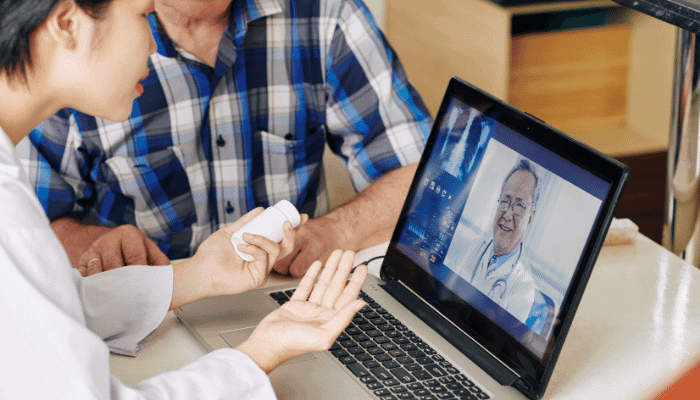
One year on from the onset of COVID-19, telemedicine has risen as an alternative, if not an exclusive means of evaluating care while staying connected with patients. Prior to the pandemic, urgent care had accounted for the majority of telehealth visits, with only one percent of global doctor appointments being conducted virtually in 2019. The Health Insurance Portability and Accountability Act (HIPAA) has long limited how identifiable health information was transmitted, effectively prohibiting the use of remote care platforms. Since the national public emergency took hold, covered healthcare providers were granted the ability to use remote communications technologies to connect with patients and expand telehealth services. With penalties for non-compliance while acting in good faith out of the question, it’s safe to say the industry has fundamentally transformed and is unlikely to ever fully return to normal.
The proof is in the numbers, with satisfaction levels for telehealth service amongst the highest of all healthcare. The J.D Power Telehealth Satisfaction Study revealed an overall score of 86 percent last October, as patients become more accustomed to improved health outcomes. While there’s the chance that new pain points will arise if HIPAA regulations shift back, providers navigating the new landscape have a valuable opportunity to learn how best they can be there for patients. In an effort to utilize man and machine assets in the most resourceful, impactful way possible, there is an ongoing need to establish the right blend between the virtual and physical across the continuum of care.
The cause for physical appointments
Diagnosis of health conditions isn’t a black-or-white scenario. We’re a long way off being able to solely rely on and trust technology to handle the process of determining treatment. Inevitably, there are elements of even the most routine check-up that can’t be conducted through video calls between patients and professionals, such as feeling for swollen glands.
Regardless of COVID-19, there’s always going to be a need for high-touch support. With the Johnson & Johnson vaccine the latest to be rolled out across the States, American life appears to be beginning to return to “normal”, but some fear it’s all too soon. There remains a concern for adults who have a higher risk of developing the illness if affected, which currently stands at approximately four in ten adults (37.6 percent). High risk populations need medication in a timely manner, and they may receive a new diagnosis that they have questions about.
As the vaccine roll-out gathers pace, so too does the distinct need for conversational Artificial Intelligence (AI) to field growing enquiries in a streamlined manner and triage patients that require human intervention. Patients want to know, “am I eligible for the vaccine?”, “how long do I have to wait for my appointment”, “what are the side effects of the vaccine?”. The mental impact on patients alone, as they try to find quick answers about the life-saving medication and deal with new variants causing a surge in infections, is placing more importance on bolstering asynchronous telemedicine. More than 42 percent of people surveyed by the U.S. Census Bureau in December reported symptoms of anxiety or depression during that month, an increase of 11 percent from the previous year. Online portals and AI-assisted chatbots that facilitate patient-provider communications are proving critical in easing this emotional burden. Performing as a consistent first point of contact, asynchronous platforms are answering frequently asked questions, helping patients decide whether to get tested for the virus, and locating healthcare facilities in the event they need to visit. For the sake of speed, convenience, and improving the safety of patients and providers alike, telehealth offers many advantages over the conventional face-to-face doctor’s visit.
A 70/30 virtual/physical approach
Telehealth services are therefore no longer considered a backup plan for traditional means of healthcare, and instead a complement to in-person care. Yes, technology enables providers to pinpoint which agents are best suited to support roles and facilitate remote training programs, but it will never have the cognitive capability to allay the evolving concerns of patients.
It doesn’t have to be all or nothing. A hybrid approach to patient care will be essential to support users across their health journey and create better clinical outcomes for millions unable or unwilling to receive in-person care. Practitioners should be maintaining that critical brick-and-mortar presence to help with specific and complex needs and keep practitioners available to deliver a truly personalized, empathetic experience. Yet, the majority of resources should be dedicated to virtual care, to capitalize on the flexibility and scalability of remote communication tools. Remote monitoring tools and telehealth visits can be used to establish whether an initial diagnosis can be given and/or the patient needs to visit the doctor’s office. Having a range of accessible high-touch and high-tech channels means providers can place more emphasis on what happens before and after each appointment to enhance the overall patient experience. Providing online forms and hosting pre-appointment video calls, for example, shaves valuable time off the patient’s journey and allows companies to maintain a continuum of care – not to mention a stronger bottom line
Will healthcare ever be “normal” again?
In a post-pandemic world, where quarantining and social distancing may no longer be the norm, an emerging hybrid model of collaborative care will empower access to care for all. As connected devices create new opportunities for quality care scale, patients are satisfied in using the technologies they already use day-to-day to source advice or next best steps in resolving healthcare issues. With the option to schedule virtual visits, with the same doctor they seen in person, and/or seek treatment in clinics, a cohesive experience is created for providers and patients alike.
Linda Comp-Noto, Divisional President of Healthcare at Teleperformance, discusses how healthcare providers are still a long way off from the post-pandemic era, and how they are establishing the right mix of telemedicine and in-person care.
The Editorial Team at Healthcare Business Today is made up of skilled healthcare writers and experts, led by our managing editor, Daniel Casciato, who has over 25 years of experience in healthcare writing. Since 1998, we have produced compelling and informative content for numerous publications, establishing ourselves as a trusted resource for health and wellness information. We offer readers access to fresh health, medicine, science, and technology developments and the latest in patient news, emphasizing how these developments affect our lives.