By Chris Jaeger
Rural hospitals are facing severe challenges in maintaining operating margin, with uncompensated care being a major factor. Telehealth eConsult platform use in local primary care settings to improve “right time, right place, right provider care” have been shown to decrease the number of patients receiving avoidable and unnecessary care within the hospital setting, thus supporting hospital’s ability to mitigate uncompensated care.
Uncompensated care is an overall measure of hospital care provided for which payment was not received from the patient or payer group. It equates to the sum of a hospital’s bad debt (+) — the financial assistance it provides. Financial assistance includes care for which hospitals never expected to be reimbursed and care provided at a reduced cost for those in need. A hospital incurs bad debt when it cannot obtain reimbursement for care provided; this happens when patients are unable to pay their bills, but do not apply for financial assistance, or are unwilling to pay their bills.
Hospitals, both nonprofit and for-profit, provide uncompensated care for individuals who are un- and underinsured.
Though there has been a noted decline in uncompensated care since the 2014 passage of the Affordable Care Act and Medicaid expansion, this has not carried over to states not part of the expansion. States that expanded Medicaid to low-income adults under the ACA recognized a 47%decrease in uncompensated care costs, on average, compared to an 11 percent decrease in states that did not expand Medicaid.
(Coverage map as of Feb 2019)
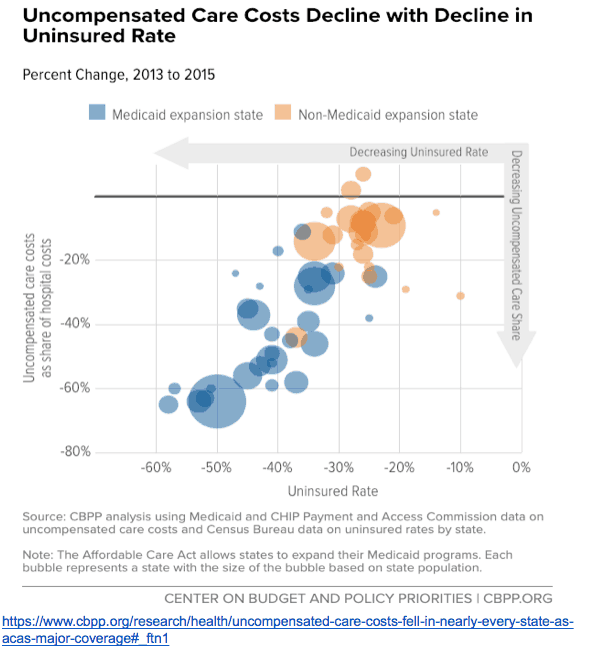
Uncompensated care and dropping revenue margins are causing hospitals, especially in rural areas, to close. “While Medicaid expansion has improved all hospitals’ operating margins and total margins, the effect was particularly pronounced in rural areas,” noted a report from the Center on Budget and Policy Priorities. A recent study by the North Carolina Rural Health Research Program (NC-RHRP) at the University of North Carolina Cecil G. Sheps Center for Health Services Research (UNC-CH) showed that since 2010, 89 rural hospitals in 26 states have closed.
Much of this uncompensated care could be prevented through primary care intervention. A report, released by Premier, found that six common chronic conditions accounted for 60 percent of 24 million Emergency Department (ED) visits in 2017; out of that 60%, approximately 1/3 of the visits (4.3 million) were likely preventable and could be treated in a less expensive outpatient setting.
More community care centers are adopting eConsult platforms that increase access to timely specialist care, from within the primary care office, to reduce unnecessary referrals and better manage total patient care. Increased access to necessary care could pose a solution to mitigate the number of patients seeking care within ED settings that is more appropriate for primary care. eConsults are a resource that has supported the reduction of up to 30% of admissions and 17.1% of readmissions. This could support for-profit hospitals in decreasing the amount of uncompensated care they are providing.
Chris Jaeger is Head of ACO and Health System Strategy for AristaMD.
The Editorial Team at Healthcare Business Today is made up of skilled healthcare writers and experts, led by our managing editor, Daniel Casciato, who has over 25 years of experience in healthcare writing. Since 1998, we have produced compelling and informative content for numerous publications, establishing ourselves as a trusted resource for health and wellness information. We offer readers access to fresh health, medicine, science, and technology developments and the latest in patient news, emphasizing how these developments affect our lives.







