Driving and sustaining tangible healthcare labor productivity improvement requires transparency, shared understanding, and end-user empowerment.
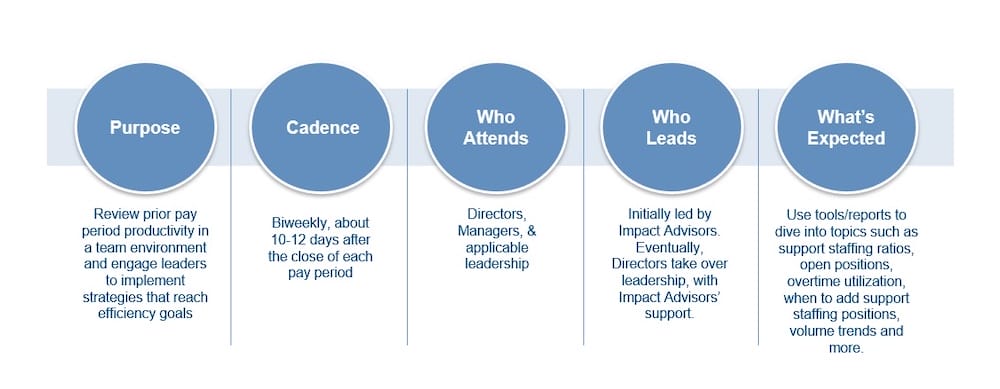
One of the cornerstones of effective labor transformation is biweekly labor productivity huddles, which serve as a platform to review prior pay period performance, understand the root cause of productivity variances, and identify solutions to mitigate those variances. This helps drive a culture of transparency and continuous improvement across the organization while creating a common language for discussing labor productivity.
Overview of Biweekly Labor Productivity Huddles
The huddle process starts by organizing staff into logical groups by department and/or related service lines (i.e., separate huddles for inpatient nursing, perioperative and ancillary services, support services, etc.). This ensures discussions are as meaningful as possible.
Managers review their biweekly labor productivity reports in advance of the meeting and identify the driver(s) of their variances. Transparency is critical, so the labor productivity reports sent to managers and C-Suite executives are the same.
During a typical huddle, the frontline manager will review the productivity report from the previous pay period with the group, talk candidly about any challenges and variances during that time, and discuss an action plan with the team to address those challenges and variances. The Service Line Lead is expected to direct the huddles, and it is important that senior leadership team members are present as well, so they can hear directly from frontline staff.
The huddle process repeats every two weeks, into perpetuity, and quickly becomes an ingrained part of the hospital’s culture, typically within a few months.
Overview of Productivity Huddles
Keys to Success
Gathering teams together every two weeks to carefully review performance from the previous pay period, candidly discuss challenges, and brainstorm on a targeted action plan helps create a common language about labor productivity across the organization. The huddles give staff a safe place to talk about their struggles, learn from their peers, and also highlight successes – which ultimately drives a culture of transparency and continuous improvement.
Effective change requires a solid foundation of customized education and training, the right data, strong executive engagement, and an organizational commitment to rigor.
- Customized education and training. Hospitals and health systems have traditionally trained frontline managers to “read” their labor reports without providing any context on how the numbers in those reports are calculated. Leaders cannot effectively manage their labor if they don’t know what factors impact their productivity metrics. Working closely with frontline managers is a priority – including as much 1:1 coaching as needed outside of the huddles – to ensure they understand not only how productivity metrics are calculated, but also the levers they can use to drive meaningful change. It’s essential that the process empowers leaders to not only understand the Worked Hours Per Unit of Service (WHPUOS), Paid Hours Per Unit of Service (PHPUOS), and Cost Per Unit of Service, but also how to effectively manage to these metrics.
Educating managers about the data in their labor reports helps them develop a “small business owner” mindset, empowering them with the understanding they need to be able to effectively communicate with their team, their supervisor, and C-Suite executives about variances.
- The right data. Data in the productivity reports needs to be current and accurate, reflecting the latest in terms of volume, salaries, and hours paid. Many hospitals use data that is 1-2 months old for their labor reports, which severely limits their ability to make any meaningful adjustments to current staffing challenges.
As a result, it’s recommended to focus on data 7-10 days after the close of the pay period, in addition to looking specifically at the data from the previous day (utilizing a tool such as a “Daily Productivity Checkbook” can help to efficiently gather this type of data). There is also charting and trending data available to help managers proactively staff for average volumes by day of the week, month, and quarter.
The data in productivity reports also needs to be aligned with organizational goals. Most hospital labor reports are based solely on Worked Hours Per Unit of Service (WHPUOS) – but that ignores the crucial element of costs. A better approach focuses on establishing labor productivity targets based on WHPUOS, Paid Hours Per Unit of Service (PHPUOS), and Cost Per Unit of Service. Improvement should be measured based on the organization’s unique historical performance, not external benchmarks.
- Strong executive engagement. A director of finance or CFO needs to be internally championing the huddles and pushing the process forward. The effort cannot be driven by an external vendor or consulting firm. If the huddles and the work required to prepare for them are not a priority for leadership, there is no reason to expect it to be a priority for frontline staff. Senior management needs to lead by example, starting with consistent attendance and active participation in the meetings.
Without continuous accountability from the highest level, there is no realistic way to sustain improvements and operationalize the action plans discussed during the huddles.
- An organizational commitment to rigor. Biweekly huddles represent a fundamental change in the way most hospitals approach productivity. The cultural shift – with leaders taking a “small business owner” mindset to managing their labor – is massive. There needs to be a commitment to rigor and a willingness for change at every level of the organization. Frontline staff need to understand the value or the “why” behind the productivity huddles from the start.
A successful approach is highly focused on empowerment and engagement. At Impact Advisors, we begin by leading the huddles, but quickly “move to the back of the room” as managers become more invested in the process and empowered to lead the discussions.
The Bottom Line
In the current environment, there is a significant opportunity and incentive for hospitals and health systems to fundamentally change the way they approach labor. One of the cornerstones of the process is biweekly productivity huddles, which help create a common language around labor productivity across the organization and drive a culture of continuous improvement.