Key Takeaways:
- USP General Chapter <800> outlines hazardous drug (HD) management standards, which are more important than ever.
- Just as hospital organizations prioritized USP General Chapter <797> in pursuit of improved patient safety, they are now widening their focus to also prioritize USP <800> to protect personnel involved in handling HDs and to promote patient and environmental protection.
- The soon-to-be-published “AIHA Hazardous Drug Surface Contamination Guidance Document” establishes frameworks and best practices for establishing HD programs that go beyond USP GC <800> compliance to continuously improve employee safety.
With assessments, controls and testing systems, healthcare organizations can establish hazardous drug programs that meet new USP <800> standards and provide high-value, lower-risk operations for patients and employees.
For nearly 50 years, the healthcare industry has grappled with a contradictory truth: If not managed properly, the drugs that save our patients’ lives can put our employees at risk.
In the early 1970s, many chemotherapy drugs were discovered to be hazardous to the healthcare employees responsible for compounding and administering them. These drugs were linked to skin rashes, hair loss, infertility, miscarriage, birth defects and even cancer.
In 1990, after years of research, the American Society of Health-System Pharmacists (ASHP) published ASHP Guidelines on Handling Hazardous Drugs, which expanded the risk beyond chemotherapy treatments to include a broad range of “hazardous drugs” (HDs). Resulting recommendations specific to HD handling from the National Institute of Occupational Safety and Health (NIOSH) provide guidance on implementing comprehensive HD programs; however, like all NIOSH publications, the guidelines are voluntary and not legally enforceable. The Occupational Safety and Health Administration (OSHA) has also provided guidance but does not have a focused, enforceable HD regulation. Some OSHA state plans, such as those for North Carolina, have developed specific regulations for HDs.
Several general OSHA regulations, including 1910.1200 Hazard Communication and 1910.132 Personal Protective Equipment (PPE), can be cited for HD handling in healthcare settings. Published in 2016, USP General Chapter <800> became a focused standard for HDs in healthcare that can be enforced by accreditation organizations.
USP <800> puts the focus on worker safety
In December 2019, United States Pharmacopeia (USP) published General Chapter <800>, “Hazardous Drugs – Handling in Healthcare Settings,” its definitive standards for the safe handling of HDs. This standard has remained informational until November 2023, when it will become enforceable. USP <800> includes standards to provide worker protections from HDs and applies to nonsterile and sterile compounding addressed respectively by USP <795>, Pharmaceutical Compounding – Nonsterile Preparations, and USP <797>, which protects patient safety.
Now the healthcare industry is just months away from a November 1, 2023 official date to adhere to the USP <800> standards. For some healthcare systems, that looming deadline is forcing organizations to sharpen their focus on employee welfare.
The challenges of USP <800> compliance
While all healthcare organizations prioritize improved worker safety, adhering to USP <800> standards has proven to be difficult due to a dynamic confluence of factors, including:
- A lack of interdisciplinary coordination and accountability. An operational chasm between pharmaceutical manufacturers and healthcare systems has contributed to inefficiencies and created room for confusion. Moreover, while health system pharmacy teams are undoubtably HD experts for patients, they cannot be solely responsible for comprehensive, enterprise-wide HD management for worker protections. Other key players such as health and safety, infection control, nursing, facilities, and environmental services need to participate in a systemwide HD program.
- USP <800> wording leaves room for interpretation. For example,
- Occupational and environmental health and safety (OEHS) professionals may define “risk assessment” in a variety of ways, while USP <800> refers to specific “assessment of risk” protocols. These terms and processes are similar, and both are focused on work task/activity evaluations. The difference is simply OEHS professionals’ language versus pharmacy professionals’ language. Both examine what HD is present during a specific HD handling activity, what control systems are in place, and what the actual risk of potential worker exposure to an HD is.
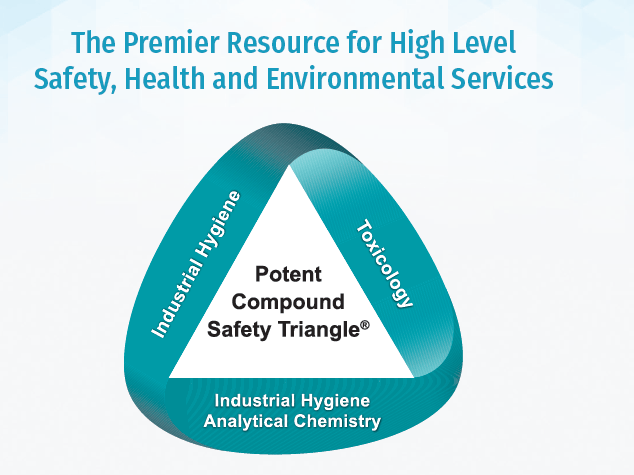
- The pharmaceutical industry has a strong framework for HD handling (aka potent compounds handling). These pharmaceutical manufacturing HD handling systems can also be implemented in a healthcare system.
- An ineffective focus on lagging indicators. Many have interpreted USP <800> largely in terms of surface contamination measurements while failing to investigate root causes. Surface contamination is a lagging indicator, one that can only demonstrate risk after an HD handling event where HD is released to the environment. Without robust control systems, engineering, administrative and personal protective equipment (PPE) controls to limit exposure, hospital systems will forever be applying bandages to achieve compliance while continuing to put their workers at risk. Proactive risk assessments (or “assessment of risk”), qualitative or quantitative (with air and surface sampling), can confirm the effectiveness of control systems and identify gaps for continuous improvement.
- Competing priorities. Many healthcare systems have already wisely invested significant time and resources into ensuring USP <797> adherence. This focus on patient safety has built systems that should also provide worker protections in the pharmacy. It is time to shift and widen the focus to include worker safety and confirm that control systems are effective for worker protections inside the pharmacy and beyond.
- Acceptable surface limits (ASLs) vary by HD. With no uniform ASL for all HDs, measurement protocols can be confusing and difficult to manage for professionals unfamiliar with setting ASLs and related occupational exposure limits (OELs).
Start here: Critical steps to establishing a high-value, effective HD program
Healthcare organizations must establish HD programs that provide effective worker protections and enable continuous improvement and sustainable compliance.
The American Industrial Hygiene Association (AIHA) has developed a comprehensive USP <800> guidance document designed to help healthcare systems focus their resources by systematically identifying gaps and prioritizing prevention with robust control systems at every point along the HD path. This upcoming publication, “AIHA Hazardous Drug Surface Contamination Guidance Document,” provides frameworks and best practices for designing and deploying an HD management system along these critical steps:
Step 1: Establish an interdisciplinary team. Engage members of the OEHS team, pharmacy, nursing, administration, risk and/or quality management. Consider bringing in external leadership support to act as a project manager. An external industrial hygienist, for example, can objectively help your team:
- Develop and implement written programs and SOPs.
- Measure exposure potential through surface and air sampling techniques.
- Establish controls to prevent potential exposure.
- Coach for best practices based on observations of routine work tasks.
- Conduct or assist with problem-solving and root-cause analysis (RCA) when HD program gaps are identified.
- Develop corrective and preventive actions (CAPA) to address gaps and confirm effectiveness and continuously improve your HD program.
Step 2: Refine your HD list per April 2023 NIOSH criteria and include ASLs for each HD. Develop a procedure to review all new drugs as they enter your formulary to determine if they are HDs per NIOSH or your system-defined criteria. An occupational toxicologist is an excellent resource that can assist with these evaluations and the development of a systematic approach to evaluate drugs that are new to your formulary.
Step 3: Navigate each HD’s path. Precisely map the journey of each HD through your organization. The USP GC <800> standard contains handling requirements from receipt through disposal, so documenting the HD path is critical to ensuring compliance and reducing risk throughout your facility and for all your health system workers.
Step 4: Communicate the HD list through your healthcare system (with focus points within the HD path) and provide custom training to minimize exposure risk. At a minimum, each department must be trained to recognize HDs, find safety data sheets (SDSs) for HD hazard information, and use control systems (engineering, administrative and PPE). Customized training programs should arm individual employees with simple ways to minimize personal risk within their day-to-day work tasks.
Step 5: Conduct risk assessments (or “assessments of risk”) in each department, including pharmacy, nursing administration, environmental services/housekeeping, and waste management, for each job function. The AIHA guidance document includes examples of controls systems that can be applied to enhance risk assessments within individual healthcare systems.
Step 6: Convert required surface sampling into a tool for continuous improvement. A positive HD surface sampling result may indicate the potential for worker exposure and the need for additional cleaning. The AIHA document suggests targeting surface sampling efforts on high-touch “sentinel” surfaces to provide insights into the effectiveness of your control systems. When surface sample results indicate issues within the controls, hospital systems should immediately conduct an RCA to identify the root cause(s) and implement CAPA to improve overall control systems and ways of working. Consider engaging an external partner to provide off-site monitoring; maintenance and emergency response planning; coordination of certification efforts; and a response to compliance issues, if they arise.
From compliance to continuous improvement
Don’t let USP <800> become just another cost of compliance. SafeBridge and Working Buildings consultants, with proven solutions, can convert USP <800> compliance into programs that continuously enhance worker safety, boost employee experiences, and ultimately improve patient outcomes.
About Trinity Consultants
Founded in 1974, Trinity Consultants began as an air quality consulting firm for industrial clients. Today Trinity provides clients across many industries with solutions in regulatory compliance, ecology and water, built environment and life sciences markets. Trinity has more than 1,400 employees in 80 offices across four continents, and partners with clients to create a sustainable and livable world across the natural and built environments.