Many medical professionals are generally unaware of the physical repercussions of compromised bite health, being also unaware of the dental occlusion’s extensive neurologic reach into and outwards from the Central Nervous System (CNS).1,2 Poor bite health induces problems far beyond the oral cavity that both patients and physicians may not realize are caused by the patient’s bite. These negative health influences are not solely tied to bite alignment, but to the actual tooth contacts themselves, and how they operate neurologically during chewing, eating, swallowing, and if the patient clenches or grinds their teeth.
Bite function compromised health conditions that frequently appear with and without apparently ideal bite alignment are3-11:
- Temporomandibular Disorders Symptoms (TMD)- Facial Pain and tension, chewing fatigue, frequent jaw soreness, reduced mouth opening, clicking, popping and locking TM joints, unilateral facial swelling, clenching and Bruxism
- Hearing Disorders – Tinnitus, Meniere’s Disease (progressive unilateral hearing loss), unexplained recurrent earache, ear fullness, vertigo, drop attacks
- Trigeminal Neuralgia – Episodic shooting or burning facial pain
- Chronic temporal headaches – Often termed “tension headache” and some migraine headaches
- Posture Anomalies – Forward Head Posture (FHP), uneven shoulder alignment, head canting
- Restricted Motion – Neck turning limitations, shoulder and arm pain, throat tightness
- Brain Fog – Episodic cloudy consciousness
- Airway constriction – A significant component of Obstructive Sleep Apnea (OSA)
- Some Ticks and Dystonias – Unexplained eye twitching, and some intermittent facial, neck and shoulder ticks are often bite related
Many of these conditions elude effective medical solutions because usually no organic disease is isolated (absent of tumors, cysts, or infections), so patients ultimately undergo “symptomatic management”. Wearing cumbersome mouthguards to keep teeth apart, physical therapy, laser therapy or acupuncture try to loosen tight muscles, repeated pain medication use, and frequent Botox injections are often employed by health care providers to lessen a patient’s suffering, with some unfortunate patients undergoing gamma knife brain surgery. But for many patients the symptoms return because these solutions do not target the underlying causation, thereby affording only temporary relief of these confounding conditions.
Computer analysis of the bite using high tech interocclusal sensors (T-Scan 10 Novus High Definition sensors, Tekscan Inc., Norwood. MA USA, www.tekscan.com/dental) and simultaneous surface electromyography (BioEMG III, Bioresearch Assoc., Milwaukee, WI. USA, BioResearch Associates) (Figures 1a and b), have isolated the main culprit of many chronic conditions as being the frictional time-durations that opposing posterior teeth push each other in and out of their sockets and bend each other on their axes from prolonged bite surface friction that occurs when teeth are functioning.3,6,12,13
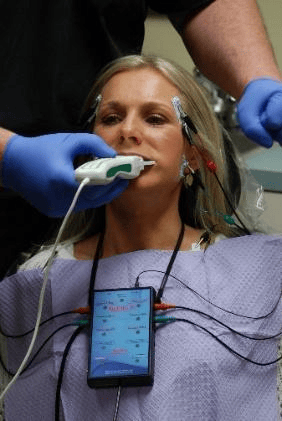
Figure 1a– The T-Scan 10/BioEMG III can simultaneously record a patients bite function and the muscular response to that bite function.

Figure 1b – The T-Scan High Definition Bite Force Sensor in the Novus recording handle that together capture changing dynamic bite forces in differing chewing movements.
This prolonged friction termed the posterior Disclusion Time3,12 when longer than 0.5 seconds duration triggers excessively long tooth pulp and Periodontal Ligament (PDL) nerve transmissions that afferently communicate directly (without an intervening synapse) with both the Trigeminal Motor Nucleus (TrMoNU) and the brain’s Reticular Formation (RetF), a major brain center that controls swallowing, sleep, posture, sexual function, circulation, and breathing (Figures 2, 3, 4).1,2 These nerve transmissions occur thousands of times per day as patients chew, eat and swallow. Once in the RetF, these posterior teeth nerves directly influence outgoing nerve transmissions to the muscles and structures associated with continuously breathing while chewing food and swallowing, ensuring food enters the digestive tract rather than the lungs. Without this specialized tooth-induced neural control, food in the airway and lungs would choke and asphyxiate humans.
The muscle groups involved are 1,2:
- Masticatory
- Submandibular
- Swallowing
- Cervical
- Facial expression
- Airway pharyngeal
- Inner ear
- Tongue, and soft palate.
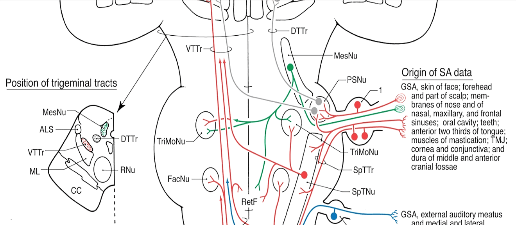
Figure 2 – The green nerve pathway emanates from molar and premolar pulp and PDL mechanoreceptors passes through the Mesencephalic Nucleus (MesNU) to synapse in the Trigeminal Motor Nucleus (TrMoNU) and with the Reticular Formation (RetF). Reprinted from Haines Neuroanatomy, 8Th Ed., Lippincott, William, and Wilkins publishers, http://lww.com)
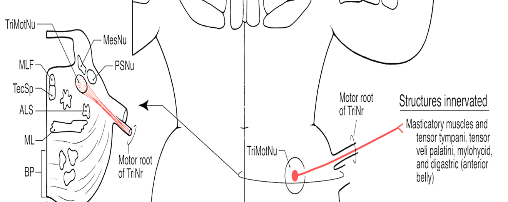
Figure 3 – The Swallow Mechanism muscles innervated by the Trigeminal Motor Nucleus (TrMoNU). Reprinted from Haines Neuroanatomy, 8Th Ed., Lippincott, William, and Wilkins publishers, http://lww.com
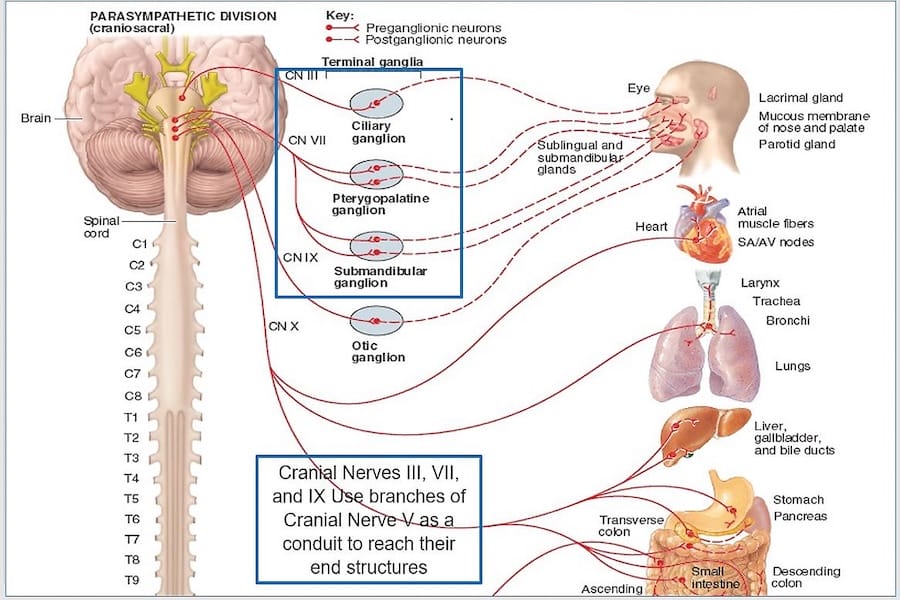
Figure 4 illustrates the extensive neural control the Trigeminal Nerve (CN V) has over chewing, swallowing, and breathing simultaneously, as CN V is used by 3 other cranial nerves (CN III, VII, IX) to reach their end structures. The posterior teeth (part of CNV, Div III) directly communicate with the center of the brain (RetF), and 4 cranial nerves to ensure food does not enter the lungs.
Figure 4 – The Trigeminal nerve aids the OculomotorTrochlear, Facial, and Glossopharyngeal nerves in reaching their end structures. Posterior tooth pulp and PDL motor fibers influence many structures that 4 cranial nerves and the RetF control. Adapted from https://quizlet.com/132746657/chapter-15-the-autonomic-nervous-system-ganglia-flash-cards/.
In some patients posterior tooth surface friction and its’ neural pathways produce excessive neurologic brain input that then hyper-contracts the muscles promoting proper foodstuff movement into digestion. This hypercontraction goes on undetected for years as teeth function normally, often with what is considered to be ideal bite alignment (Figures 5 and 6). Lactic acid pooling in the involved muscles blocks oxygen uptake resulting in pain, constriction and reduced functionality, which cannot be detected with MRI, CBCT, or radiographic imaging, thereby eluding an accurate diagnosis. Although the dental occlusion is well known to provide sensory feedback to the CNS, the occlusion’s motor component emanating from each posterior tooth’s pulp and Periodontal Ligament (PDL) is widely misunderstood, yet causes many muscular dysfunctional symptoms with no detectable organic causation.
Figure 5 – The apparently ideal bite alignment of a chronic pain patient with face, head and neck painful muscle groups.
Figure 6 – Despite the visually ideal alignment in Figure 5, this patient’s left chewing movement has definitive posterior tooth friction that triggers excess neural input to the CNS.

Figure 7 – The same patient’s left chewing movement’s T-Scan 10/BioEMG data Desktop with prolonged posterior tooth contacts (left pane T-Scan data) that elevate muscle activity in the left temporalis, and bilateral masseter muscles (yellow box; after the C line in the top EMG pane). This hyperactivity creates long-term lactic acid build-up and chronic muscle dysfunction.
But prolonged Disclusion Time can be shortened down to <0.5 seconds per chewing movement with computer-guided high-precision bite adjustments, to create very little muscle activity within the same chewing movements. Short Disclusion Time results in posterior teeth missing each other instead of frictionally rubbing together6,7,12, that directly lessens the volume of muscle activity, neurologically controlling the amount that inputs into the brain. What then emanates from the Reticular Formation and on 4 cranial nerves is the least hyper-activating muscle contractions needed to perform chewing and swallowing. Disclusion Time Reduction (DTR) therapy neurophysiologically stops the ongoing process of lactic acid accumulation, which is metabolized away from the involved muscles (for the first time in many years), so patient symptoms rapidly decline as oxygen reenters each muscle allowing fibers to heal and strengthen. Multiple computer-guided high precision bite treatment studies have repeatedly shown chronic pain patients demonstrate physical and emotional improvements in one to three months following initial DTR therapy.3-16 Importantly, treating the dental occlusion resolves many conditions from within the CNS, rather than failing to resolve these same conditions externally to the CNS using repeated symptomatic management methods.3-16
An example of the physical removal of excess muscle activity from the masticatory muscles can be seen in Figures 8-12.
Figure 8 – A pre-operative fully intercuspated occlusion with relatively ideal bite alignment
Figure 9 – The right chewing movement has all posterior teeth in prolonged frictional contact which transmits excessive neural stimulation into the CNS.
Figure 10 – The middle of the right chewing movement T-Scan/BioEMG III data showing right posterior forces (T-Scan data left pane) hyperactivating muscle activity levels in the right temporalis (242.9 uv) and both masseter muscles (MM-R = 284.1 uv; MM-L = 138.5 uv) (top 2 right EMG panes). Note all the contractile waveforms visible inside the yellow box. The pre-treatment right chewing Disclusion Time = 3.73 seconds.
Figure 11 – Bonding the right canine and then adjusting away the surface friction from the right chewing movement with DTR therapy created visible posterior tooth separation not apparent in Figure 9
Figure 12 – Post computer-guided DTR bite treatment, the right chewing Disclusion Time was lessened to = 0.35 seconds, which is 10x shorter than pretreatment, markedly lessening the right chewing muscle activity levels ( right temporalis = 55.2 uv, right masseter = 9.8 uv; left masseter = 4.7 uv). Note the lack of contractile waveforms visible inside the yellow box.
This patient now chews right using very low muscle contraction levels, allowing for both less lactic acid pooling and its’ metabolism, which is followed by fiber reoxygenation and improved chewing strength.16,17 This relaxation phenomenon also occurs in the other head, neck and pharyngeal muscles that neurologically control swallowing food, breathing at the same time, and moving food into the digestive tract rather than the lungs.
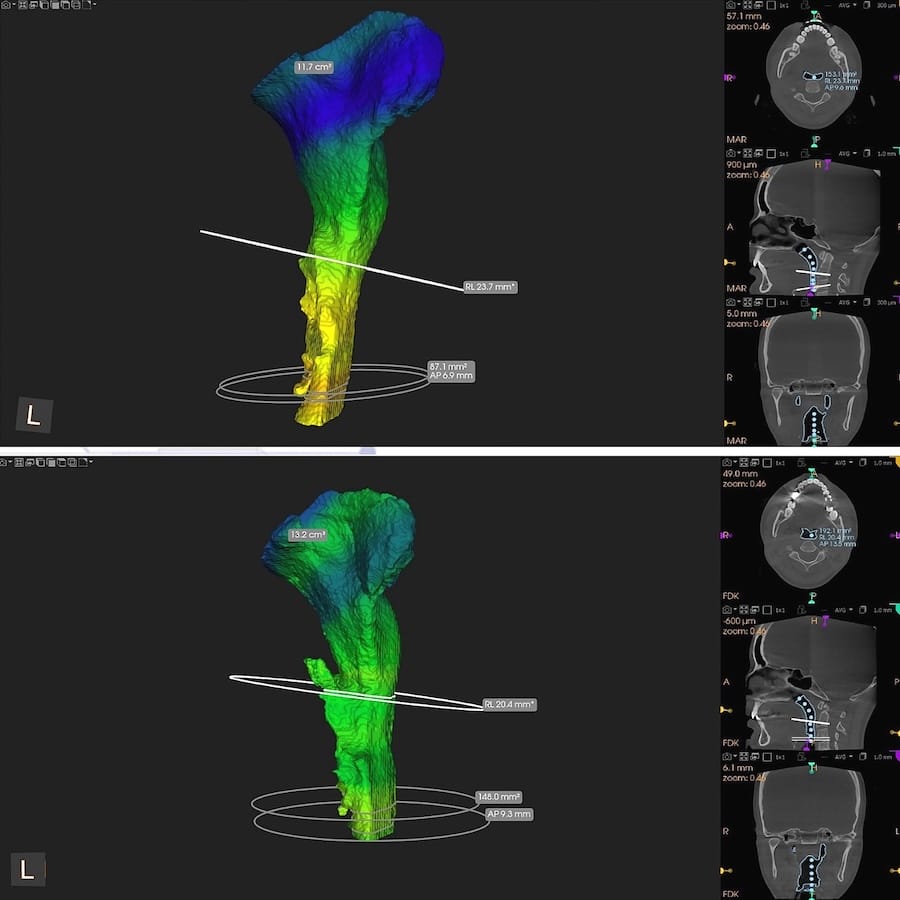
This same physiological response of changing the Disclusion Time from long to short can widen the airway constriction of a sleep apnea patient who wears a nighttime sleep appliance that forces his jaws apart, attempting to open his airway (Figures 13 and 14).11
Figure 13 – A CBCT comparison of airway volumes pre (top pane) to post Disclusion Time Reduction (bottom pane). A much wider airway followed the DTR-induced pharyngeal muscle relaxation (pre DTR Volume = 100.5 mm2; post DTR volume = 157.1 mm2). Note the post DTR airway is more parallel walled without being conically constricted pre-treatment.
Figure 14 – The airway constrictions compared pre (top pane) to post DTR (bottom pane) illustrate the patient’s airway widened following DTR. By gaining 57 mm2 of airway volume, this patient no longer needed his sleep appliance, slept more soundly, and experienced less apneic episodes.
Its important to understand that these profoundly interconnected neuroanatomic pathways emanating from the molar and premolar teeth can often misdirect treatment based on the patient’s presentation. An example is when someone describes “zygomatic arch pain”, which is frequently perceived by physicians and dentists as “sinus pain and pressure”. The provider then prescribes an antibiotic, despite that the clinical exam reveals the patient’s sinuses appear clear, their nose appears clear, they’re not experiencing a stuffy or runny nose, nor are they frequently sneezing. Although the patient is describing “painful cheek bones”, what they are actually experiencing is masseter muscle pain from lactic acid accumulation occurring at the zygomatic arch that is hurting over the maxillary sinus. A T-Scan 10/BioEMG III analysis would likely isolate masseter hyperactivity and prolonged bite friction, which with computer guided DTR bite treatment could stop the pain by removing lactic acid. Without understanding the occlusion’s extensive neuroanatomic reach, one may not realize the patient’s “sinus pain” was actually caused by their bite function.
Disclusion Time Reduction (DTR) is a high-precision bite adjustment procedure that treats fictional chewing contact durations that can only be detected with the T-Scan 10 technology. DTR quickly reduces masticatory and swallow muscle hyperactivity with significant supportive literature validating DTR’s effectiveness in treating myogenous TMDs.3-17 However, the documented benefits of DTR go well beyond treating TMD patients, because of the far reaching neural outreach of the dental occlusion’s neuroanatomy.1,2,8-11 The next time a chronic pain patient seeks a physician’s help for strange, chronic, episodic and recurrent muscular postural symptoms with no detected organic etiology, one should consider the dental occlusion as a very likely cause.
References
1. Haines, D.E. (2012). Neuroanatomy. An atlas of structures, sections, and systems, Ed.8, Baltimore, MD: Lippincott, Williams, & Wilkins. pp 199, 227.
2. https://quizlet.com/132746657/chapter-15-the-autonomic-nervous-system-ganglia-flash-cards/.
3. Uchale, P., Deogade, S., Khalikar, A., Wankhade, S., Taneja, S., & Lalsare, S. (2024). Effectiveness of T-Scan technology in identifying occlusal interferences and its role in the management of Temporomandibular Disorders: A Systematic Review. Journal of Clinical and Diagnostic Research, 18(6), ZC09-ZC15 DOI: 10.7860/JCDR/2024/67960.19470
4. Thumati, P., Poovani, S., Bharathi, B., Mounika, A., Kerstein, R.B., & Radke, J. (2020). A Disclusion Time Reduction Randomized Controlled Occlusal Adjustment Trial. Advanced Dental Technologies and Techniques, 2,1-23.
5. Thumati. P., Thumati, R.P., Kerstein, R.B, & Radke, J. (2021). Bruxism Improvements After Disclusion Time Reduction (DTR) – A Pilot Study. Advanced Dental Technologies & Techniques, 30, 54-64 Epub
6. Kerstein, R.B., & Radke, J. (2012). Masseter and temporalis excursive hyperactivity decreased by measured anterior guidance development. Journal of Craniomandibular Practice, 30(4), 243-254.
7. Thumati. P., Thumati, R.P., Poovani, S., Sattur, A., Srinivas, S., Kerstein, R.B., & Radke, J.A. (2021). Multi-Center Disclusion Time Reduction (DTR) Randomized Controlled Occlusal Adjustment Study Using Occlusal Force and Timing Sensors Synchronized with Muscle Physiology Sensors. Sensors, 21, 23, 7804 https://doi.org/10.3390/s21237804
8. Sutter, B.A, Thumati, P., Thumati, R.P., & Radke J. (2022). Meniere’s Disease Patients Treated with Disclusion Time Reduction (DTR): A Retrospective Cohort Study of 86 Patients (Part 1 of 4). Advanced Dental Technologies & Techniques, 5(1), 10-22. ePub
9. Thumati, P., Thumati, R.P., Kerstein, R.B., & Radke, J. (2020). Trigeminal Neuralgia Improvements After the Immediate Complete Anterior Guidance Development Coronoplasty (ICAGD). Advanced Dental Technologies & Techniques, 4(2), 66-75. Epub.
10. Sutter, B.A., & Girouard, P. (2021). Posture Stability and Forward Head Posture Before and After Disclusion Time Reduction. (DTR). A Five-Year Cohort Study. Advanced Dental Technologies & Techniques, 3(2), 23-35. Epub.
11. Sattur, A. (2024) .Airway Volume Changes Detected by Cone Beam Computed Tomography (CBCT) in Muscular Temporomandibular Dysfunction Patients Treated with Disclusion Time Reduction (DTR) Therapy. In, T-Scan Technology Applications in Dental Medicine. IGI Global, Hershey, PA, pp 1477- 1592.
12. Kerstein, R.B., & Wright, N. (1991). An electromyographic and computer analysis of patients suffering from chronic myofascial pain dysfunction syndrome, pre and post – treatment with immediate complete anterior guidance development. Journal of Prosthetic Dentistry, 66(5), 677- 686.
13. Qadeer, S., Ozcan, M., Edelhoff, D., & van Pelt, H. (2020). Accuracy, reliability and clinical implications of static compared to quantifiable occlusal indicators: a literature review. European Journal of Prosthodontics and Restorative Dentistry, 28, 1-12.
14. Thumati. P., Sutter, B., Kerstein, R. B., Yiannios, N. & Radke, J. (2018). Changes in the Beck Depression Inventory – II Scores of TMD Subjects after Measured Occlusal Treatment. Advanced Dental Technologies & Techniques, 1(1), 1-13.
15. Kerstein, R.B., & Radke, J. (2006). The effect of Disclusion Time Reduction on maximal clench muscle activity level. Journal of Craniomandibular Practice, 24, 3, 156-165.
16. Kerstein, R.B., & Radke, J. (2017): Average chewing pattern improvements following Disclusion Time Reduction. CRANIO® 35, 135-51. DOI:10.1080/08869634.2016.1190526
17. Kerstein, R.B., & Radke, J. (2019). Computer-guided Occlusal Treatment Improves Smoothness, Timing and Velocity of Gum Chewing. Advanced Dental Technologies & Techniques, 1(2), 11-21.

Robert B. Kerstein, DMD
Dr. Robert B. Kerstein received his D.M.D. degree in 1983, and his Prosthodontic certificate in 1985, both from Tufts University School of Dental Medicine. From 1985 - 1998, he maintained an active appointment at Tufts as a clinical professor teaching Fixed and Removable Prosthodontics. In 1984, Dr. Kerstein began studying the original T Scan I technology, and has since that time has also studied T-Scan II, T-Scan III, T-Scan VII, T-Scan 8, T-Scan 9, and now the present-day version, the T-Scan 10 Novus technology.
Over the past 40 years, Dr. Kerstein has published many original research studies using all versions of the T Scan, that has led to his becoming the leading authority and researcher in the field of Computerized Occlusal Analysis. His findings have been published in many journals including the Journal of Prosthetic Dentistry, the Journal of Craniomandibular and Sleep Practice, Quintessence International, Practical Periodontics and Aesthetic Dentistry and the Journal of Computerized Dentistry. Additionally, Dr. Kerstein has edited 9 research volumes about all the known applications of the T-Scan Computerized Occlusal Analysis technology.A pioneer and academic science advocate for digital occlusal technology, Dr. Kerstein teaches a measured system which greatly improves the success of bite-related procedures commonplace in every dental practice. Digital Measured Occlusion provides predictable, rapid bite comfort for most patients, while lessening prosthesis breakage and remakes and shortening treatment times.