By Thanh Tran, CEO, Zoeticx, Inc. and Dr. Donald Voltz, Aultman Hospital, and David Conejo, CEO, Rehoboth McKinley Christian Health Care Services
The Center of Medicaid and Medicare Service (CMS) continues to increase emphasis on care collaboration, ranging from Chronic Care Management (CCM) to the recent announcement from the US Surgeon General’s landmark report on alcohol, drug and health. Derived from many aspects in healthcare, the authors’ examine the challenges of integrating physical and behavioral healthcare, addressing the Care Collaboration Model outlined by CMS and the Surgeon General.
Interdependency Between Mental and Other Chronic Disorders
Research has demonstrated bidirectional links between mental disorders and chronic conditions. Depression and anxiety are heightening the risks towards hypertension and diabetes along with other mental disorders such as PTSD, drug addiction and alcoholism. Depression roughly doubles the risk for a new Coronary Heart Disease (CHD) event. Such interdependencies have limited solutions today due to the lack of a collaborative environment. We refer to this as a ‘revolving door care environment’, a vicious cycle compounding the effects of chronic and mental disorders.
A detox center can only retain the patient for detoxification for a limited time. Without collaborating with other behavioral services, the patient will inevitably return to the same habit – either drug addiction or alcoholism. Depression can stem from a social environment or from a recently developed chronic condition such as CHD.
The primary care provider will continue to address the chronic condition without the knowledge of what may actually feed into the patient’s chronic condition. It is yet another ‘revolving door’ for the physical care environment. Such interdependency requires a care collaborative environment between care providers.
Care Collaborative Model and Bidirectional Information Flow
A team-based care collaborative model uses a multidiscipline group of care providers supporting and implementing treatment with the patient at the center. A bidirectional information flow is an absolute must to put the model into realization and operation in healthcare institutes.
Today, healthcare lacks the support of a closed-loop system, one that emphasizes a bi-directional flow of information. Healthcare is muddled with reactive care, instead of preventive, anticipated care. It is that lack of prevention and anticipation that have an adverse impact on the overall healthcare cost and patient outcomes. EHR and EMR systems are the main ‘anchors’ of today’s health IT.
However, there are two EHR components that are non-starters: the boundary of the health institute and unidirectional systems. HIEs (Health Information Exchange) address EHR limitations with their capability to provide support across health institutes, but actually worsen the unidirectional character of the EHR. Neither EHR or HIE can address the requirements for a care collaborative model.
Hospital system CEOs and CIOs need to look at this issue carefully. This IT issue offers health care facilities the perfect opportunity to not only promote the care collaborative model, but offer a solution to resolving the bidirectional information flow problem and enable them to move forward with a new platform to achieve better patient outcomes, the goal of all healthcare facilities.
Reaching The State of Homeostasis As A Desired Patient Outcome
The objective is to improve patient outcomes, but how do you define a patient’s outcome?
Homeostasis is a biological term, referring to the stability, balance, or equilibrium within the body. Homeostasis is the process of maintaining a constant internal environment by providing the body with what is needed to survive for the well being of the whole. While disorders (physical or mental) reflect the abnormal condition of the body, homeostasis is the normal, stable and well-being state.
Each disorder is well documented with what would be a normal condition or the state of homeostasis. This state of homeostasis also deviates based on race, demographics, and above all, the relationship with other existing disorders afflicting the patient. It is then noted that each patient outcome requires a personalized state of homeostasis.
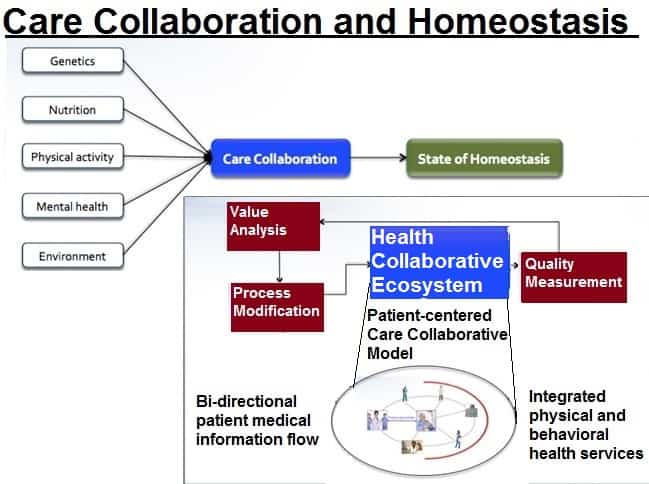
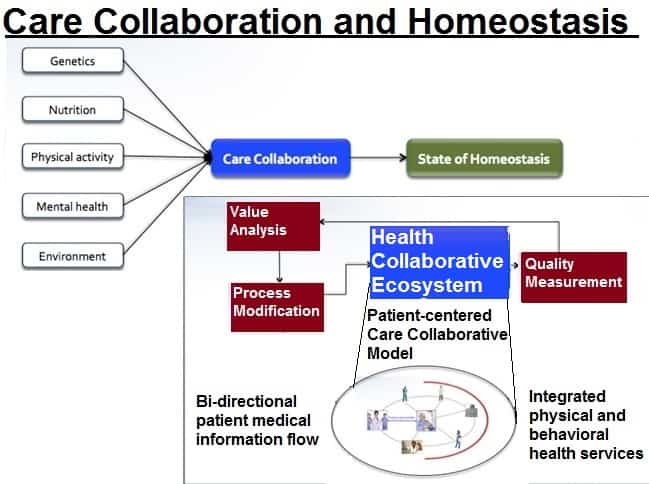
From the disorder, the process towards the state of homeostasis consists of genetics, nutrition, physical activity, mental health and an external environment. Genetics is the internal influencer in with medicine’s physical care plays a role in adjusting the disorder toward homeostasis. For healthcare, it is the care plan for a disorder.
The state of homeostasis should be used as the measure of a patient’s outcome, resulting from the care collaborative model addressing the integrated, coordinated care from multiple care providers.
Health Collaborative Ecosystem
The Health Collaborative Ecosystem is the delivery process that supports the care collaborative model, with the objective of bringing the patient to the state of homeostasis. This system would include all providers of health-related services to the chronically ill patient diagnosed with one or more of the designated chronic and debilitating diagnosis that utilize the most significant percentage of health care spending. Such a system would be:
- Capable of integrating physical and mental care environments.
- An integrated layer complementing (including EHR-agnostic) existing health IT infrastructures, supporting care activities beyond the brick and mortal walls of their facility or clinic.
- Consensus among providers to standards of care and bidirectional information flow that encourages innovation, compliance with regulations, secures privacy and adopts a continuous process of improvements to better reach a patient’s state of homeostasis.
Why an Ecosystem?
- An Ecosystem is a collective system, including a health IT solution and consulting guidance, and support, for hospital operations in order to maximize the benefits of care collaboration, through efficiency and scalability of a care providers’ bandwidth.
- It is an Ecosystem because it must include an auditable compliance component to provide crucial measurements and enforce quality guidelines for the model according to hospital and clinic management.
- It is an Ecosystem because it must include the ability to track and monitor progress towards the state of homeostasis for all attributes contributing the patient’s overall well being.
Case scenarios
As noted in one case study, Maria Viera, age 75, takes a dozen medications to treat her diabetes, high blood pressure, mild congestive heart failure, and arthritis. After she begins to have trouble remembering to take her pills, she and her husband visit her primary care physician to discuss this and a list of other worrisome developments, including hip and knee pain, dizziness, low blood sugar, and a recent fall. Maria’s primary care doctor spends as much time with her as he dares, knowing that every extra minute will put him further behind schedule. Yet despite his efforts, there is not enough time to address her myriad ailments. She sees several specialists, but no one talks to all her providers about her care, which means she may now be dealing with conflicting recommendations for treatment, or medications that could interact harmfully. As a result, Maria is at high risk for avoidable complications and potentially preventable emergency department visits and hospital stays.
The care team for the above patient would potentially consists of: a primary care provider (high blood pressure and care coordinator), a cardiologist (congestion heart failure), an endocrinologist (diabetes), dietician (diabetes), a rheumatologist (arthritis), physical and/or occupational therapists (arthritis, falls, hip and knee pain), and a psychologist or a psychiatrist (depression).
The above case brings challenges to the health care system on multiple fronts:
- More time from primary care providers with limited result outcomes due to the lack of collaboration with other care providers, specialists and community services.
- Potential conflicting recommendations for treatment due to the lack of coordination and bidirectional medical information flows from multiple care providers and specialists.
- The patient’s risk for complications, emergency visits and hospital stays significantly increases.
- As conditions worsen, the patient develops symptoms for behavioral health conditions.
Today’s solution for the above scenario is based on care management. The care manager would work with all care providers, manually “pulling and pushing” the patient’s medical conditions and updates to all involved care providers. Error prone, high cost, and low efficiency are some of today’s deficiencies for healthcare attempts in implementing the care collaborative model, outlined by CMS.
Net New Revenue Focusing on Preventive Care
This is the challenge of a ‘revolving door care environment’ in addressing the need for integration between physical and behavioral health services. The Health Collaborative Ecosystem is the answer for such a challenge.
However, to support such a revolution, healthcare, as an industry, needs to have the financial incentives. As stated in the introduction of this paper, CMS is now encouraging a transformation through financial incentives.
The authors’ propose a roadmap to roll out the Health Collaborative Ecosystem without upfront risks and budget planning, but to generate new revenue for the institutes. The implementation roadmap leverages these CMS initiatives:
- Annual wellness visits
- Chronic care management
- Integration of physical and behavioral health through the care collaboration model
With the Health Collaborative Ecosystem’s objective is to create a patient state of homeostasis, rural and community hospitals and clinics can accomplish multiple goals – better services to the community, better defined patient outcomes and open new avenues for health services with behavioral health and filling the revenue gap.
The Editorial Team at Healthcare Business Today is made up of skilled healthcare writers and experts, led by our managing editor, Daniel Casciato, who has over 25 years of experience in healthcare writing. Since 1998, we have produced compelling and informative content for numerous publications, establishing ourselves as a trusted resource for health and wellness information. We offer readers access to fresh health, medicine, science, and technology developments and the latest in patient news, emphasizing how these developments affect our lives.