By Stacey Lang, Senior VP, Corazon, Inc.
Healthcare leaders today face exceptional challenges in planning for organizational growth and/or sustainability. In fact, in some cases, just sustaining the current situation can be difficult, without even attempting any growth. Surely, uncertainty regarding reimbursement, evolving treatment trends, and the need to be maximally efficient in care delivery all combine to make effective and realistic strategic planning essential for future viability in any service line. However, in neurosciences in particular, this is especially significant due to the associated costs with respect to manpower and capital equipment as well as in ensuring staff training and competency for this complex and diverse patient population.
For many years, neuroscience clinical offerings were viewed as exclusively within the purview of tertiary, quaternary, or academic medical centers. But, due to clinical advances, the escalating needs of an aging population, and the availability of integrated technology solutions, select neuroscience service offerings are now often appearing in the community hospital setting. This then becomes a chief concern of strategic planning efforts, as regardless of hospital size or scope, Corazon believes that a clear, well-thought-out plan for the development of neurosciences is an absolute necessity.
An effective neuroscience strategic planning effort must begin with the end in mind. Understanding current capabilities as well as organizational and system goals for 3, 5, and even 10 years into the future is necessary given the complexity, expense, and infrastructure requirements of neuroscience programs.
Corazon suggests the following areas of focus in order to ensure a realistic and achievable strategic plan.
Assess Current Capabilities at a Regional Level
“Population health management” and “networks of care” are not just hot industry buzz phrases. A regional approach to planning and care delivery is essential for success in todays’ competitive healthcare landscape. This is perhaps nowhere more important than in the area of neurosciences, as this specialty encompasses a wide array of diagnosis and treatment requirements across both medical and surgical specialties. The integration of endovascular capabilities over the past decade adds an additional layer of complexity to the distribution of services across a community or region as well as within individual health systems or organizations.
Further, the significant capital investments required for the implementation of some tertiary services, as well as a typical lack of foundational neuroscience clinical expertise in community hospitals, can mean that attempts to integrate full neuroscience capabilities will not be successful. Rather than an “all things to all people” approach, the exploration of partnering options and the development of integrated networks of care across a geographic area is often the better solution.
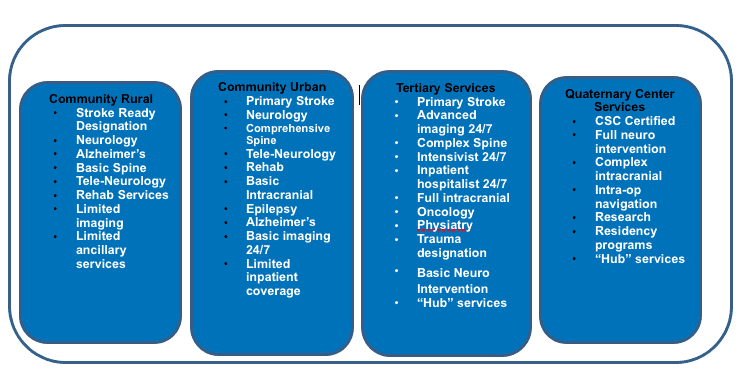
Corazon recommends that an objective internal assessment of existing capabilities be undertaken as a first step. Once accomplished, a similar exercise to assess regional capabilities within a 60-mile radius will allow a full understanding of both potential challenges to considered service expansion as well as opportunities related to discrete service offerings that are identified as underutilized. Corazon categorizes neuroscience offerings into 4 categories in order to assist in this evaluation process:
Community Rural providers are typically those organizations of 100 to 150 beds with limited physician and radiology capabilities. In-house neuro expertise may be limited or non-existent and ancillary areas are not in service on a 24/7 basis. Most commonly these hospitals are “spoke” organizations in the hub and spoke model of stroke care.
Community Urban providers are hospitals with greater than 150 beds, a more robust infrastructure and existing basic in-house neuroscience expertise. These organizations often have tertiary partner agreements in place for the transfer of advanced neuro-interventional patients or for those who require open heart surgery, for example. Community Urban providers may already have Level II trauma designation in place as well.
Tertiary Service Providers typically are larger centers with greater than 200 licensed beds. These organizations routinely treat higher-acuity patients in other disciplines, and so typically benefit from the infrastructure already in place with respect to critical care medicine, hospitalist support, and 24/7/365 diagnostic testing and ancillary support. Tertiary service providers usually possess full neuroscience capabilities but may have additional needs related to cost containment, LOS management, and a patient population with consistently higher-than-average acuity.
Quaternary Service Providers are most commonly academic medical centers with a robust infrastructure and full service offerings in both pediatric and adult neuroscience. These organizations integrate research activities into care delivery and have the benefit of active residency programs and comprehensive in-house neuroscience expertise.
Neuroscience Service Capabilities
Push the Envelope
Achieving an understanding of existing capabilities, both internal and external, is a vital step in establishing clear and achievable goals and expectations for a strategic planning process. When considering an expansion of neuroscience service offerings, it is essential that leaders be willing to not only focus on what is, but also on what could be. The rapid adoption of tele-medicine by many organizations across the country has, in many ways, been a driver of the delivery of more complex care in a community setting. In the case of stroke for example, the ability to rapidly diagnose and provide thrombolytics to patients in the community setting was not even considered 20 years ago. Today, through this approach, patients are being treated and treated well in their own communities with transfer only being necessary for those requiring intervention.
In much the same way, select intracranial procedures, complex spinal procedures, and discrete medical neurology diagnoses can be integrated into available services in many community hospitals to the benefit of all involved. Adopting a programmatic approach to services already in place, in many cases, brings an immediate benefit with respect to incremental revenue capture and an expansion of staff capabilities. Understanding what is already in place that can be built upon, as well as the future direction of clinical capabilities in those existing services, can serve to clearly define where an organization should place focus.
Case Study
In July 2009, Corazon was engaged to assist with the implementation of a Primary Stroke Center program at a small community hospital in the mid-atlantic region. This organization had been acquired by a large system several years earlier. At that time, the hospital was an under-utilized community hospital of 246 beds with an average daily census of 85 that lacked a definitive clinical identity. Although the hospital was recognized as a “high-touch” facility with caring staff, it was not recognized within the community as a leader in the provision of clinically complex and/or technology-dependent healthcare services. Prior to acquisition, the hospital had struggled financially and was unable to fund the capital investments necessary for both facility and equipment upgrades.
In order to ensure patient safety, promote quality outcomes, and maintain patient and staff satisfaction, a staged approach to the possible implementation of full neuroscience capabilities was adopted. The key clinical offerings in order of projected implementation were as follows:
- Primary Stroke Program
- Expanded Spine Capabilities
- Neuroscience Intensive Care Unit
- “Low risk” Intracranial (i.e., Deep Brain Stimulation Procedures)
- Intracranial Neurosurgery: (i.e., Tumor Resection)
- Neuro Endovascular Capabilities
- Neurovascular Neurosurgical Capabilities
Following a two month planning process, the strategic plan was completed and approved by the Board. Over the next 24 months, the services noted above were implemented. The program demonstrated excellent clinical quality and patient satisfaction rates in excess of 95%.
Conclusion
The experience at this hospital perfectly illustrates the benefit of an organized, thoughtful, and comprehensive approach to the planning and development of a neuroscience center of excellence. Through a thorough understanding of market needs, the securing of necessary financial and expert clinical resources upfront, and informed, involved senior leadership, it was possible to develop full neuroscience capabilities on the heels of certification as a primary stroke center within the span of just two years.
Corazon offers consulting, recruitment, interim management, and information technology services to hospitals and practices in the heart, vascular, neuro, and orthopedics specialties. Find Corazon on facebook at www.facebook.com/corazoninc or on LinkedIn at www.linkedin.com/company/corazon-inc. To learn more, call 412-364-8200 or visit www.corazoninc.com. To reach the author, email [email protected].
The Editorial Team at Healthcare Business Today is made up of skilled healthcare writers and experts, led by our managing editor, Daniel Casciato, who has over 25 years of experience in healthcare writing. Since 1998, we have produced compelling and informative content for numerous publications, establishing ourselves as a trusted resource for health and wellness information. We offer readers access to fresh health, medicine, science, and technology developments and the latest in patient news, emphasizing how these developments affect our lives.








