As the Executive Director of the Physician-Patient Alliance for Health & Safety, a non-profit whose mission is the improvement of patient safety, I am often asked how to tell a “good” hospital (i.e. patient safe) from a “bad” hospital (i.e. unsafe).
In thinking about “good” and “bad” hospital leadership, I am reminded of two discussions I had with hospital leaders – which leaders’ hospital would you rather be a patient at or, if you are a clinician, work at?
I spoke with the CEO of a hospital, who was dealing with the family of a child that had died within the hospital from opioid-induced respiratory depression. His clinicians had not employed continuous electronic monitoring with pulse oximetry for oxygenation or with capnography for adequacy of ventilation. The Physician-Patient Alliance for Health & Safety encourages the continuous electronic monitoring of all patients receiving opioids:
To improve patient safety and save patients’ lives, we recommend adopting continuous respiratory monitoring of all patients receiving opioids with pulse oximetry for oxygenation and with capnography for adequacy of ventilation to improve timely recognition of respiratory depression, decompensation or clinical deterioration.
Hearing this, I pleaded with him to implement continuous electronic monitoring. In addition, to countering the bad press his hospital was receiving and the resulting loss of patients and revenues (which seemed more his concern), I offered to have medical and advocacy leaders, including myself, stand on the doors of his hospital (after he had made changes) and endorse his hospital’s commitment to patient safety. He resolutely refused to make these changes, believing that he and his clinicians had acted appropriately, and was reluctant to meet with the family.
In another conversation at a large hospital chain, the Quality and Safety Officer told me that on the occurrence of any adverse event or death, a SWAT team of administrators and clinicians immediately start identifying what had happened and speaking with the patient and family. This SWAT team is then responsible for implementing any necessary changes in hospital procedures.
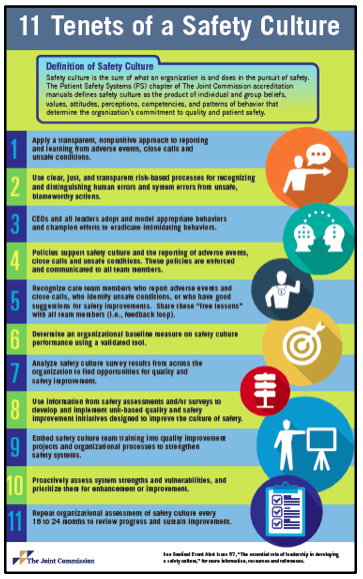
Leadership throughout the hospital – whether at the executive level, in the ICU, or in a nursing unit – affects the organization, its people, its patients, and its visitors. The Joint Commission in its most recent Sentinel Event Alert, “The essential role of leadership in developing a safety culture”, reminds us of the role of leaders by placing patient safety squarely on their shoulders:
In any health care organization, leadership’s first priority is to be accountable for effective care while protecting the safety of patients, employees, and visitors. Competent and thoughtful leaders* contribute to improvements in safety and organizational culture. They understand that systemic flaws exist and each step in a care process has the potential for failure simply because humans make mistakes …
The Joint Commission’s Sentinel Event Database reveals that leadership’s failure to create an effective safety culture is a contributing factor to many types of adverse events – from wrong site surgery to delays in treatment. In addition, through the results of its safety initiatives, The Joint Commission Center for Transforming Healthcare has found inadequate safety culture to be a significant contributing factor to adverse outcomes. Inadequate leadership can contribute to adverse events in various ways, including but not limited to these examples:
- Insufficient support of patient safety event reporting
- Lack of feedback or response to staff and others who report safety vulnerabilities
- Allowing intimidation of staff who report events
- Refusing to consistently prioritize and implement safety recommendations
- Not addressing staff burnout
This is a powerful reminder that leaders must set the tone for their organizations from the executive level, as well as in units and teams within the clinical setting, otherwise adverse events and patient deaths may ensue.
My discussions with the CEO and the Quality and Safety Officer illustrate the difference between “highly reliable” organizations (HROs) and those that are not. In their article “High-Reliability Health Care: Getting There from Here”, The Joint Commission President and CEO Mark R. Chassin, M.D., M.P.H., and executive vice president for healthcare quality evaluation Jerod M. Loeb, Ph.D. say:
HROs have “an environment of ‘collective mindfulness’ in which all workers look for, and report, small problems or unsafe conditions before they pose a substantial risk to the organization and when they are easy to fix. These organizations rarely, if ever, have significant accidents. They prize the identification of errors and close calls for the lessons they can extract from a careful analysis of what occurred before these events. These lessons point to specific weaknesses in safety protocols or procedures that can be remedied to reduce the risk of future failures.”
Although we would like to think that our hospitals are HROs and are more like that of the Quality and Safety Officer and less like that of the CEO, the reality may be the reverse. Chassin and Loeb discuss this unfortunate reality:
How close or far away is the typical hospital today from this state of high reliability? The answer is, quite far. In health care, we rarely observe the five principles of high reliability guiding the actions of organizations, their leaders, and caregivers. As opposed to a preoccupation with avoiding failure, hospitals, and other health care organizations behave as if they accept failure as an inevitable feature of their daily work.
In thinking about my discussions with the CEO and the Quality and Safety Officer, two things strike me.
The first is an observation of process and protocols. One of the main goals of my meeting with the Quality and Safety Officer was the use of the PCA Safety Checklist in his hospital. The PCA Safety Checklist was developed with a group of 19 renowned health experts and provides recommended steps when initiating and continuing patient-controlled analgesia (PCA).
The Quality and Safety Officer and I discussed how one mark of a “good” hospital is safety protocols, which often take the form of a checklist. In their research, “Implementation of checklists in health care; learning from high-reliability organisations” Øyvind Thomassen and his colleagues write about the role of checklists in HROs:
“Checklists are commonly used in HROs as cognitive aids, freeing mental capacity for the operation itself. These organisations have decades of experience with checklist development and implementation.”
The second is that processes are really only as good as the people who implement them. In the hospital of the Quality and Safety Officer, there is a culture of safety (the “people” factor) and an accepted process for ensuring that the goal of safety is continually pursued (a checklist, for example). So, in regard to the PCA Safety Checklist, we discussed how the Checklist ensures essential steps are observed. However, a culture of safety relies upon the intervention and judgment of clinicians. For example, if continued PCA administration might lead to respiratory compromise, the intervention of a clinician is needed to adjust medication selection or dosing.
Dr. Atul Gawande, who is the author the Checklist Manifesto, and was part of the expert panel for the development of the PCA Safety Checklist, discussed this juxtaposition of process and people as follows:
“the real lesson is that under conditions of true complexity—where the knowledge required exceeds that of any individual and unpredictability reigns—efforts to dictate every step from the center will fail. People need room to act and adapt. Yet they cannot succeed as isolated individuals, either—that is anarchy. Instead, they require a seemingly contradictory mix of freedom and expectation—expectation to coordinate, for example, and also to measure progress toward common goals.”
However, in thinking about my discussions with the CEO and the Quality and Safety Officer, “good” leadership goes beyond the adherence to protocols and checklists. There is also a stark contrast in attitude. On the one hand, the Quality and Safety Officer sees each adverse event and death as a learning process. He wants to know what happened and to learn whether there are improvements that could be made. He trusts the people around him and believes the SWAT team will be able to perform both of these tasks. Moreover, he wants to share this with the patient and family involved. On the other hand, the CEO takes a completely defensive posture. There is no desire to learn from what happened or to improve on existing practices. Moreover, there is no desire to engage the patient or family.
So, how can you tell the difference between a “good” hospital and a “bad” one?
If you are a patient (and we are all be patients, whether we are clinicians or not), there are hospital safety scores out there, such as the LeapFrog Hospital Safety Grade which allows users to look up a hospital and see how well that hospital is graded. For better or worse, these grades are limited to “how safe they keep their patients from errors, injuries, accidents, and infections.”
And, if you are a hospital leader, The Joint Commission has set forth 11 steps to achieve a patient safe culture:
So, the next time I am asked the question – “How can you tell a ‘good’ (i.e. patient safe) hospital from a “bad” (i.e. unsafe) hospital?” – I can answer, just look to its leaders and see whether they are patient safe.
Michael Wong, JD is Executive Director for the Physician-Patient Alliance for Health & Safety.







1 thought on ““Good” Hospitals Require Real Leaders”
Comments are closed.